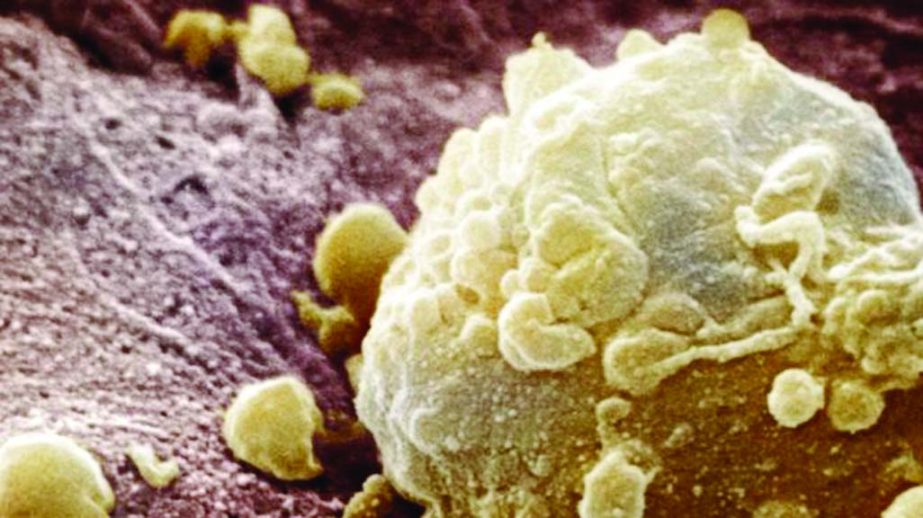
BBC Online :A pair of cancer drugs can shrink tumours in nearly 60% of people with advanced melanoma, a new trial has suggested.An international trial on 945 patients found treatment with ipilimumab and nivolumab stopped the cancer advancing for nearly a year in 58% of cases.UK doctors presented the data at the American Society of Clinical Oncology.Cancer Research UK said the drugs deliver a “powerful punch” against one of the most aggressive forms of cancer.Melanoma, the most serious form of skin cancer, is the sixth most common cancer in the UK – it kills more than 2,000 people in Britain each year.Harnessing the immune system is a rapidly developing field in cancer research.The immune system is a powerful defence against infection. However, there are many “brakes” built in to stop the system attacking our own tissues.Cancer-which is a corrupted version of healthy tissue – can take advantage of these brakes to evade assault from the immune system. Ipilimumab, which was approved as an advanced melanoma treatment by the UK’s health service last year, and nivolumab both take the brakes off.An international trial on 945 people showed that taking both drugs led to tumours shrinking by at least a third in 58% of patients – with the tumours stable or shrinking for an average of 11.5 months.The figures, published simultaneously in the New England Journal of Medicine, for ipilimumab on its own were 19% and 2.5 months.Dr James Larkin, a consultant at the Royal Marsden Hospital and one of the UK’s lead investigators, told BBC News: “By giving these drugs together you are effectively taking two brakes off the immune system rather than one so the immune system is able to recognise tumours it wasn’t previously recognising and react to that and destroy them.”For immunotherapies, we’ve never seen tumour shrinkage rates over 50% so that’s very significant to see. “This is a treatment modality that I think is going to have a big future for the treatment of cancer.”The first analysis of the data received top billing at the cancer conference in Chicago, but the key piece of information – how long treated patients live – is still unknown.”We hope these early responses will turn out to be durable, but at the moment we can’t say,” said Dr Larkin.Side-effects such as fatigue, a rash or diarrhoea are also an issue. More than half of those tested had side effects on combination therapy compared to around a quarter on ipilimumab alone.It is also uncertain why some people responded exceptionally well to treatment, while others had no benefit at all.Dr Alan Worsley, Cancer Research UK’s senior science information officer, said: “This research suggests that we could give a powerful one-two punch against advanced melanoma by combining immunotherapy treatments.”Together these drugs could release the brakes on the immune system while blocking cancer’s ability to hide from it.”But combining these treatments also increases the likelihood of potentially quite severe side effects.”Identifying which patients are most likely to benefit will be key to bringing our best weapons to bear against the disease.”Ipilimumab is given intravenously every three months and costs around £100,000 for a year. Nivolumab is given every two weeks until it stops working. Both drugs were developed by Bristol-Myers Squibb.Many pharmaceutical companies are developing similar drugs that have the same effect on the immune system. Pembrolizumab, by Merck, is another leader in the field.But the great hope is these immunotherapies will prove to be effective treatments for a wide range of cancer types.Cait Chalwin, 43, from Cornwall, started the trail after she was diagnosed with melanoma in 2013.A growth on her face that had been classed as benign was in fact cancerous and had spread to her lungs. Doctors said she had 18-24 months to live.She was treated at The Royal Marsden and her cancer is now stable, but has had to come off the trial due to side effects. She said: “I am feeling absolutely amazing now. “It took a long time to get back to normal, to feel how I felt before diagnosis, however I do firmly believe that if the treatment hadn’t worked, I wouldn’t be here now.”